|
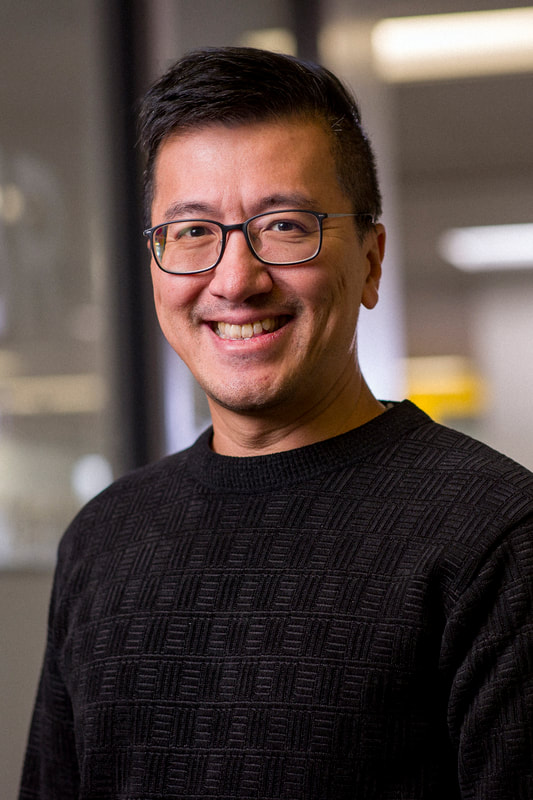
As a Principal Investigator and Director of Native American Research and the Electroencephalography Core for LIBR, Dr. Evan White, Ph.D. dedicates much of his professional effort to working with American Indian communities to advance mental health. The focus of his work is employing clinical neuroscience to improve mental health outcomes among AI communities—in particular, his research looks at two things: cultural engagement and the role it may play in providing protection against poor mental health outcomes; he also works to identify the signatures of those cultural protective factors that may enhance culturally informed prevention and intervention efforts. How does your work help advance health equity? What are you seeing in the American Indian communities? In the scope of mental health studies, our work is very much in the early stages. Unfortunately, many mental health disparities among American Indian (AI) populations remain and are potentially even growing. We have not observed changes in health disparities attributable to the research we’re doing; however, this work is advancing health equity in important ways. Native populations are vastly underrepresented in clinical neuroscience research, particularly as a population of focus. We are working to remedy this by placing AI communities at the center of our clinical-cultural neuroscience research, and by building community partnerships to collaborate in our research process. The broader goal is to incorporate principles from community-engaged research methods (Community-Based Participatory Research/CBPR in particular) whenever possible. It’s important to note that this endeavor is not unique to our research, and encouragingly, our research is informed by a substantial and growing body of health equity researchers who champion community-grounded health equity research. What are your research goals, purpose and aim? My research aims to establish and advance a neuroscientific understanding of cultural factors that are protective against poor mental health among American Indians (AI) utilizing a strength-based framework. My goal is to integrate clinical and cultural neuroscience to identify modifiable factors as candidate treatment targets for mental health intervention and prevention. We are working to establish a clinical-cultural-neuroscience framework in which mental health intervention and prevention efforts are culturally grounded, community-engaged, and guided by neuroscience. You are an enrolled member of the Absentee Shawnee Tribe of Oklahoma. Does your identity as a tribal member inspire you to research minority health, health disparities, and health equity? Improving the health and wellbeing of the populations we serve is a motivation many researchers share, and my commitment to helping the community I come from is no exception. However, my motivation extends to other communities and populations that also experience disparities and it is my hope that our work can make a meaningful impact at home and more broadly. In the scientific and medical communities, it is a well-known fact that minority communities are disproportionately impacted by mental health risk factors and, as a result, mental health conditions. Like many native people, I have seen first-hand the impacts of suicide, substance misuse, and addiction. As health disparities researchers we can play an important role in helping to address these conditions. On a positive note, I have also seen the incredible strengths and resilience of Native people and communities rooted in relationships and traditional cultural practices and values. I believe this is a critically important area for mental health disparities research – a community-grounded understanding of treating and preventing disparate mental health conditions which leverages and elevates the strengths that exist within communities. Are there any studies you’re recruiting for right now? What type of volunteers do you need? Are volunteers paid, and what’s involved in being a volunteer? We are always interested in people willing to participate in our research studies. Individuals who participate are compensated for their time and can expect to answer questions related to their health and general life experiences. If individuals qualify for one of our studies based on a variety of factors, they may be contacted to complete some additional protocols that include interviews, computer tasks and even brain scanning. This is a big question: How do we encourage the next generation of scientists? I know that for me, I received encouragement to pursue my passion from supportive mentors, training programs, colleagues, and family and friends outside of academia. The support I am given helps me find ways to encourage the next generation of scientists. We need to engage students with hands-on research opportunities early in their training—and not just data collection and curation—but also with idea development, generating research questions, analytic training, and opportunities to share and present findings with a broad audience. Providing training like this in an inclusive and growth-oriented environment allows trainees to explore and develop their own passions for research. We have created these experiences at LIBR in recent years with the LIBR Accelerated Summer Research Internship and Diversity, Research, and Mental Health Neuroscience (DReaM-Neuro) fellowship programs.
0 Comments
To coincide with Mental Health Awareness Month this May, LIBR would like to share a few key highlights from a lecture on the the State of Mental Health in 2024 presented by Dr. Martin Paulus, Scientific Director and President to LIBR scientific staff earlier in the year.
Q: What are the main challenges in global mental health systems, and what changes are urgently needed? A: Global mental health systems face significant challenges, including being under-resourced and often failing to provide adequate, quality care. There is an urgent need for systemic change, which involves shifting towards community-based care, strengthening health systems, securing political commitment, increasing financing, and leveraging digital technologies to enhance mental health services. Q: How prevalent are mental health issues in the U.S., and what are the barriers to accessing care? A: Mental health issues are widespread in the U.S., with over 50 million adults experiencing them, akin to the combined populations of New York and Florida. Despite this, more than half of these individuals do not receive treatment due to high costs and lack of insurance. Nearly 30% of adults with mental illness cannot seek treatment due to affordability issues, highlighting a critical gap in mental health care. Q: Why is a personalized approach crucial in treating depression? A: Depression manifests in varied forms and severities, influenced by a mix of individual risk and resilience factors. A personalized approach is crucial as it ensures that treatment is tailored to each person’s unique experiences, preferences, and life context, leading to more effective recovery. Involving individuals with lived experience in care decisions also enhances accountability and the efficacy of healthcare systems. Q: At what ages do psychiatric disorders typically onset, and what are the implications for mental health services? A: Psychiatric disorders often onset early, with one-third starting before age 14 and about half by age 18. This underscores the importance of early intervention and integrating mental health promotion and prevention into schools, colleges, and healthcare settings. Mental health services should support integrated care models for transitional age groups, ensuring continuous care without age thresholds. Q: How do risk and protective factors influence depression, and what strategies can be used for prevention? A: Risk factors for depression include significant life changes such as widowhood, childhood abuse, and poor physical health, while protective factors include a healthy diet rich in zinc, tea, and fruits. Strategies for prevention should address these varied factors comprehensively, helping healthcare professionals identify high-risk individuals and customize interventions to prevent or mitigate depression. Q: How do work-from-home trends and social isolation impact mental health? A: Work-from-home trends have increased, with 34% of people working from home in 2022. While this can offer flexibility, it may also contribute to social isolation and loneliness, which are linked to higher risks of premature death, heart disease, stroke, anxiety, depression, and dementia. Reducing social isolation by fostering community involvement and social connections is crucial for improving mental health. Q: What integrated solutions are recommended to address mental health challenges effectively? A: Integrated solutions include implementing early screening programs, promoting healthier living and working environments, increasing investment in mental health resources, and fostering social connections. Additionally, employing evidence-based methodologies to monitor treatment outcomes and conducting public awareness campaigns to change perceptions around mental health can significantly improve mental health care and support. April is Alcohol Awareness Month, a time to raise awareness of alcohol use and misuse. Some of LIBR’s work delves into how alcohol use affects mental health, and we are passionate about using our findings to learn more about causes and treatments. We reached out to Dr. Robin Aupperle, LIBR Principal Investigator, and Elisabeth Akeman, Licensed Professional Counselor and Lead Therapist and Clinical Research Coordinator in the Aupperle Lab, to share their knowledge about how alcohol affects the brain and mental health, how to know how much alcohol is too much, ways to reduce alcohol consumption, where to seek professional help and how LIBR is contributing to research on alcohol use.
Does alcohol use impact mental health? Absolutely – there is a complex relationship between alcohol use and mental health, as alcohol use can influence our thoughts, behaviors, and emotions. This may be especially problematic for those who tend to experience symptoms of anxiety and depression. When we experience intense negative emotions, it can be tempting to do things, such as using alcohol, to push away, minimize, or avoid those negative thoughts and emotions. Alcohol use may cause a temporary decrease in anxiety and negative emotions or even a temporary increase in positive emotions, which reinforces its use and leads people to use alcohol more frequently and at higher doses. This is an effect referred to as positive reinforcement. Continued use can prevent people from seeking out more adaptive ways of coping with negative emotions or negative life events – thus contributing to worse mental health in the long-term. In addition, chronic alcohol use can lead to changes in the brain that contribute to reductions in the experience of positive emotions and worsening of mental health. In addition, alcohol withdrawal (experienced when someone who has been using alcohol chronically quits using the drug) can lead to symptoms of anxiety, irritability, decreased mood, in addition to physical withdrawal symptoms. Individuals then may start using alcohol again to avoid these symptoms – which is referred to as negative reinforcement. In summary, the use of alcohol is often reinforced in the short-term by temporary reductions in negative emotions, while chronic or excessive use often leads to worse mental health. How does alcohol impact your brain? Alcohol affects the brain in a multitude of ways with both short- and long-term effects. Alcohol acts as a depressant, inhibiting neurotransmission and leading to decreased attention, drowsiness, and mood and memory alterations that occur when using alcohol. Alcohol is also thought to suppress inhibitory neurotransmitter systems, which contributes to reductions in social inhibitions. At higher levels, alcohol can cause acute confusion, sensory impairment, and even coma or death. Heavy and long-term alcohol use can also cause memory, attention, and processing speed issues. These effects may relate to the impact of alcohol on prefrontal “executive” systems as well as medial temporal lobe memory systems. However, these cognitive functions improve again for most people after long periods of abstinence. Alcohol also impacts the motivational systems of the brain in a way that contributes to continued use and impacts mental health. Alcohol use leads to temporary increases in neurotransmitters involved in the experience of reward, including dopamine and opioid neurotransmitters. Chronic and excessive alcohol use is thought to “hijack” the brain’s reward system such that it does not respond as much to other more natural rewards (e.g., social connection). This can lead to less engagement with these natural reinforcers and further use of alcohol to get that experience of reward or positive emotions. How do I know if I’m drinking too much? Alcohol consumption is associated with a variety of short- and long-term health risks. Risks may be related to safety (e.g., motor vehicle crashes, violence, sexual risk behaviors, etc.), as well as physical health consequences (e.g., high blood pressure, types of cancer, etc.). To reduce the risk of alcohol-related harms, the CDC recommends that adults drink in moderation by limiting intake to 2 drinks or less in a day for men or 1 drink or less in a day for women, on days when alcohol is consumed. In addition to mental and physical health risks, it is important to consider how you feel that your alcohol use is serving you and how it does or does not meet your expectations. While some may report short-term positive consequences of alcohol use (e.g., I feel less anxious), sometimes the long-term consequences of use may not be as helpful (e.g., I am late to work the morning after drinking). To help determine how alcohol is serving you, ask yourself the following questions:
What can I do instead of drinking? Alcohol use can lead us to not being present in our lives in the way that we would like to and even lead to withdrawing or avoiding certain things. This can ultimately get in the way of us living in line with our values and achieving our goals. When decreasing alcohol use, it is important to get engaged in our lives again! The best way to do this is to choose to do things that are important to YOU and that you notice have a positive impact on your mood. Re-discover your hobbies, surround yourself with friends and family, and engage in healthy self-care activities. Changing behaviors, especially those which may be more problematic, can be difficult and take a lot of effort. Setbacks are common but can be learned from. Start with small, manageable steps that lead you closer to living your most meaningful life. Don’t forget to celebrate your progress! I need help with my drinking. What resources are available? If you would like to reduce or quit drinking, don’t do it alone. Regardless of your level of intake prior to reducing, it is important to surround yourself with a variety of resources. Informal sources of support, such as friends and family, are as critical as formal sources of support (e.g., evidence-based therapy, medication, mutual support groups, etc.). A variety of resources at both local and national levels exist to support you on your journey. Rethinking Drinking, provided by the National Institute on Alcohol Abuse and Alcoholism (NIAAA), is a great place to start as it provides education, tools, and lists of resources. Reducing or quitting drinking may lead to physical, cognitive, and emotional symptoms, with rare cases leading to more severe symptoms requiring immediate medical attention. Call 911 or present to a local emergency room if you or someone you know is experiencing withdrawal symptoms. How is LIBR contributing to research related to alcohol use? Dr. Robin Aupperle, the NeuroCATT Lab team are collaborating with researchers at the University of California, San Diego (Dr. Charles Taylor) and University of California, Los Angeles (Dr. Kate Wolitzky-Taylor) on research related to the treatment of problematic alcohol use. The study is examining the impact of a novel psychotherapy intervention focused on increasing the experience of positive emotions for individuals who are experiencing problematic alcohol use as well as symptoms of anxiety or depression. Results from a previous pilot feasibility study and case series can be accessed here. The NeuroCATT Lab is recruiting participants for the ongoing randomized clinical trial with the new psychotherapy intervention. Those interested in participating can learn more about this and other studies by visiting our website www.laureateinstitute.org. To find out if you are eligible to participate, you may sign up here https://www.laureateinstitute.org/ongoing-studies. *Photo Credit: Clay Behavioral Health Center Research from Dr. Nick Obradovich and colleagues evaluating the effects of climate change on the expression of positive and negative emotions is part of news feature article published today in a Nature News Feature focused on the rise of eco-anxiety (a chronic fear of environmental doom) resulting from devastating weather-related events such as hurricanes, droughts, floods and fires. Highlighted in an associated Nature Editorial, Dr. Obradovich has also been involved in working to develop global mental-health indicators that can be linked to weather and climate data, as part of the Lancet Countdown on Health and Climate Change, that will contribute to efforts to better evaluate and effectively reduce the effect of climate change's mental health burden.
Dr. Paul Holtzheimer - April 2, 2024
"Mechanosensitive Potassium Channels in Nerves: Molecular Mechanisms, Disease Relevance, and Potential Targets for Neuromodulation" William K. Warren, Jr. Frontiers in Neuroscience Lecture 12:00 pm - 1:00 pm Program in the LPCH auditorium Dr. Steve Brohawn is an Associate Professor at the University of California, Berkeley in the Department of Molecular and Cell Biology and the Helen Wills Neuroscience Institute. Research in his laboratory is focused on understanding the molecular basis of sensory transduction and electrical signaling in the nervous system. To this end, the lab uses a combination of cryo-electron microscopy and electrophysiology to investigate the structure and function of membrane protein ion channels and transporters. Prior to starting his laboratory in 2016, Dr. Brohawn was a Helen Hay Whitney Postdoctoral Fellow in Dr. Rod MacKinnon’s lab at the Rockefeller University from 2010 to 2015 where he studied ion channels that sense mechanical force. Steve received his PhD in Biology in 2010 from the Massachusetts Institute of Technology where he worked with Dr. Thomas Schwartz on the structure and function of the nuclear pore complex. He received his B.S. from the University of Delaware in 2004 where he worked with Dr. Colin Thorpe on the enzymology of oxidative protein folding. Work in his lab has been recognized with a NIH New Innovator Award, a New York Stem Cell Neuroscience Investigator Award, a Sloan Research Fellowship, a McKnight Neuroscience Scholar Award, and a Klingenstein-Simons Research Fellowship. Learning objectives:
Saint Francis Health System designates this live activity for a maximum of 1 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity. For Psychologists: The Oklahoma State Board of Examiners of Psychologists, the American Psychological Association and the Oklahoma Psychological Association recognize AMA PRA Category 1 credit™. Saint Francis Health System is accredited by the OSMA For Social Workers: An application has been sent to the Oklahoma State Board of Licensed Social Workers for 1 hour Category 1 Clinical. For CADCs and LADCs Saint Francis Health System is accredited as a provider of continuing education programs for CADCs and LADCs through the Oklahoma Board of Licensed Alcohol and Drug Counselors. (1 hour) The LPC/LMFT This event as been approved by the State Board of Behavioral Health Licensure (BBHL) for 1 hour of CE. For questions , email: Lauren Haguewood at [email protected] In 2023, LIBR investigators published over 120 peer-reviewed research articles. In conjunction with the release of our annual report, we asked each principal investigator to weigh-in on their lab's highlights over the past year. Here's a snapshot of some of the outstanding accomplishments:
Robin Aupperle The NeuroCATT lab received an R34 award from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) in collaboration with Dr. Charles Taylor at the University of California San Diego and Dr. Kate Wolitzky-Taylor at the University of California Los Angeles. The grant will fund work furthering the development of an intervention focused on amplification of the positive valence system and reducing alcohol use (AMP-A) for individuals with alcohol use disorder and symptoms of anxiety or depression. The first phase of the project involved collecting input from substance use providers and prior participants concerning the intervention and piloting the treatment with eight individuals. This will lead into a randomized clinical trial comparing the novel intervention with a more traditional cognitive-behavioral therapy intervention. Chun-Chieh Fan Dr. Fan was invited to moderate a panel on the genomic analysis of the human brain data at the American Society of Human Genetics held in Washington, D.C, published a special issue on genetic data from the Adolescent Brain Cognitive Development Study in Behavior Genetics and was invited to give a workshop on geospatial dat analysis at the BERTHA summer school in Denmark. Salvador Guinjoan Dr. Guinjoan’s lab completed the recruitment of 20 persons who suffer from major depression and varying degrees of rumination intensity, and expect to complete recruitment of 10 persons who are healthy and will serve as a comparison group for the low-intensity focused ultrasound (LIFU) pilot study targeting white matter tracts in the anterior limb of the internal capsule in the right brain hemisphere. The lab observed consistent target engagement with this method in a preliminary analysis, and a trend towards resulting clinical effects. This was the first time that white matter tract functional modulation had been demonstrated with a noninvasive method such as LIFU, which before was only possible with costly, invasive, and risky methods involving electrode implantation or tissue ablation. This observation will allow for the testing of additional participants with the goal to make causal inferences about brain mechanisms of symptom generation in major depression and other psychiatric disorders. Maria Ironside Dr. Ironside was awarded a $2.1 million 5-year R01 grant from the National Institute of Mental Health to investigate “Processes and circuitry underlying threat sensitivity as a treatment target for comorbid anxiety and depression.” The study employs a pharmaco-fMRI approach to study threat sensitivity using a novel predator task in patients with major depressive disorder (MDD), anxiety disorders (AD), and comorbid MDD and AD. The ultimate aim of this work is to establish treatment targets for comorbid MDD and AD for novel interventions and provide evidence for the separation of MDD from comorbid MDD and AD in future clinical trials. Sahib Khalsa An ingestible vibrating capsule produced reliable changes in gastric-evoked brain activity and stomach sensation in healthy individuals. This minimally invasive mechanosensory approach serves as the basis for an ongoing NIH-funded study focused on identifying abnormal gut-brain interactions in women with anorexia nervosa as well as in individuals with functional gastrointestinal disorders. Martin Paulus Many computational measures have poor psychometric properties, which could invalidate previous findings and hinder ongoing research. The Paulus lab recommended steps to address these issues and facilitate the translation of computational assays to clinical practice. As well, Individuals with MDD have lower expression of miR-93, which is associated with higher levels of certain inflammatory markers. Unlike healthy individuals, those with MDD don’t show an adaptive epigenetic regulation of a brain region (insula) involved in processing internal body signals, hinting at the molecular mechanisms that might be altering brain responsivity to these signals in MDD. Jonathan Savitz Dr. Savitz continued his work with cytomegalovirus (CMV). Drs. Haixia Zheng and Savitz published a paper in Molecular Psychiatry showing that CMV infection is associated with suicide, increased expression of inflammatory markers and microglial “activation” postmortem. As well, the Savitz lab published a Hot Topics paper on herpesviruses and psychiatric disorders in Neuropsychopharmacology. Ryan Smith Dr. Smith began data collection on a new pilot study examining computational mechanisms of breathing perception in anxiety disorders. His lab also continued to make progress on a 3-year project funded by a grant from the Well-being for Planet Earth Foundation. This project investigates neurocomputational predictors of subjective well-being. Data collection was also completed for a study examining the influence of an interoception-based anxiety induction on decision-making mechanisms associated with information-seeking and planning. Jennifer Stewart Compared to individuals with a history of major depressive disorder (MDD) and healthy controls, individuals with amphetamine use disorder 1) report greater positive and negative urgency (taking rash action when feeling good or bad); and 2) exhibit greater right hemisphere brain signals (in right anterior/middle insula, amygdala, and ventral striatum) during successful behavioral inhibition. These findings point to heightened impulsivity during emotional arousal and recruitment of more brain resources to exert inhibitory control. Wes Thompson Dr. Thompson gave a talk at the Joint Statistical Meetings on August 7, 2023, on “Annotation-Informed Polyvertex Scores for Brain-Wide Association Studies", served as the managing guest editor for a special issue of Developmental Cognitive Neuroscience on novel methods for population neuroscience, and continued his efforts as Director of Biostatistics for three national consortia on longitudinal neurodevelopment: the National Consortium of Alcohol and Neurodevelopment in Adolescence (NCANDA), the Adolescent Brain Cognitive Development (ABCD) Study℠, and the HEALthy Brain Child Development (HBCD) Study. Evan White LIBR received a DP1 grant for research to be conducted by Dr. White in collaboration with the Shawnee Tribe of Oklahoma titled “Kipiyecipakiciipe – Coming Home: Establishing clinical cultural neuroscience as a tool for understanding the role of traditional cultural engagement in mitigating substance misuse and disorder.” Within American Indian (AI) populations, there is a disproportionate share of negative health and social consequences of substance use disorder (SUD) even after decades of awareness and research. This project aims to integrate community-based participatory research (CBPR) with neuroscience tools to examine the influence of traditional cultural engagement on resilience factors that may protect against poor mental health as well as risk for substance use. The 2023 Laureate Institute for Brain Research (LIBR) Annual Report is now available to download via the link below. The report provides an overview of last year’s happenings at LIBR, including a letter from the President and Scientific Director, Dr. Martin Paulus, information on our mission, history and specific aims, current areas of research, funding sources, events and lectures, awards, individual laboratories, select publications and opportunities to participate in research. We hope you enjoy the publication and look forward to continuing our goal to improve mental health through neuroscience in 2024 and beyond.
Dr. Paul Holtzheimer - April 2, 2024
“Transcranial Magnetic Stimulation for Psychiatric Disorders” William K. Warren, Jr. Frontiers in Neuroscience Lecture 12:00 pm - 1:00 pm Zoom Join Zoom Meeting https://laureateinstitute-org.zoom.us/j/87343165038 Meeting ID: 873 4316 5038 Passcode: 490646 Paul Holtzheimer, MD, is the Deputy Director for Research at the National Center for Posttraumatic Stress Disorder. He is Professor of Psychiatry and Surgery at the Geisel School of Medicine at Dartmouth, and a staff psychiatrist at Dartmouth-Hitchcock Medical Center and the White River Junction VA Medical Center. Dr. Holtzheimer’s clinical and research interests include developing better interventions for PTSD, depression and related disorders, especially for patients with treatment-resistant and comorbid illness. He has expertise in brain imaging and brain stimulation therapies (including transcranial magnetic stimulation, electroconvulsive therapy, vagus nerve stimulation, and deep brain stimulation). A primary aim of his research program is to better understand the neural circuitry of treatment-resistant psychiatric disorders and to use this information to develop and advance novel treatment approaches, with a particular emphasis on focal brain stimulation therapies. Dr. Holtzheimer is an author on over 100 publications in psychiatry, neurology, neurosurgery and neuroimaging. He has received research funding from the National Institutes of Health, the Department of Veterans Affairs and multiple non-profit foundations. He has served on the Council of the Society of Biological Psychiatry and on the Board of Directors for the Anxiety and Depression Association of America. He is a Fellow of the American College of Neuropsychopharmacology. Learning objectives:
Saint Francis Health System designates this live activity for a maximum of 1 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity. For Psychologists: The Oklahoma State Board of Examiners of Psychologists, the American Psychological Association and the Oklahoma Psychological Association recognize AMA PRA Category 1 credit™. Saint Francis Health System is accredited by the OSMA For Social Workers: An application has been sent to the Oklahoma State Board of Licensed Social Workers for 1 hour Category 1 Clinical. For CADCs and LADCs Saint Francis Health System is accredited as a provider of continuing education programs for CADCs and LADCs through the Oklahoma Board of Licensed Alcohol and Drug Counselors. (1 hour) The LPC/LMFT This event as been approved by the State Board of Behavioral Health Licensure (BBHL) for 1 hour of CE. For questions , email: Lauren Haguewood at [email protected] Dr. Karmel Choi - March 5, 2024
Title: Data-Driven Discovery for Preventing Depression and Promoting Resilience William K. Warren, Jr. Frontiers in Neuroscience Lecture 12:00 pm - 1:00 pm CST Program in the LPCH auditorium Karmel Choi is an Assistant Professor at Harvard Medical School/Massachusetts General Hospital (MGH) and Director of the Precision Prevention Program in the MGH Center for Precision Psychiatry. Her lab leverages tools from statistical genetics, data science, and epidemiology to understand how people show resilience in the face of risk and adversity and identify strategies for preventing stress-related disorders such as depression and PTSD. She completed her Ph.D. in Clinical Psychology at Duke University and clinical internship at Massachusetts General Hospital. Learning objectives:
Saint Francis Health System designates this live activity for a maximum of 1 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity. For Psychologists: The Oklahoma State Board of Examiners of Psychologists, the American Psychological Association and the Oklahoma Psychological Association recognize AMA PRA Category 1 credit™. Saint Francis Health System is accredited by the OSMA For Social Workers: An application has been sent to the Oklahoma State Board of Licensed Social Workers for 1 hour Category 1 Clinical. For CADCs and LADCs Saint Francis Health System is accredited as a provider of continuing education programs for CADCs and LADCs through the Oklahoma Board of Licensed Alcohol and Drug Counselors. (1 hour) The LPC/LMFT This event as been approved by the State Board of Behavioral Health Licensure (BBHL) for 1 hour of CE. For questions , email: Lauren Haguewood at [email protected] Dr. Sahib Khalsa, M.D., Ph.D., is Director of Clinical Operations for LIBR, Associate Professor at the Oxley College of Health Sciences at the University of Tulsa, Director at LIBR Float Clinic and Research Center, and Volunteer Faculty Member in the Department of Psychiatry at the University of Oklahoma. Dr. Khalsa’s laboratory studies the role of the brain-body connection in human health; he has published more than 90 peer-reviewed papers and has received research funding from the National Institute of Mental Health (NIMH), National Institute for General Medical Sciences (NIGMS), National Center for Complementary and Integrative Health (NCCIH), the NIH/National Center for Advancing Translational Science (NCATS), the Mind and Life Foundation, and the Brain and Behavior Research Foundation. His research is currently funded by NIMH and LIBR.
Q: The Laureate Psychiatric Hospital and LIBR are known and respected for their work in the fields of identifying, treating, and researching eating disorders like anorexia nervosa; as February is focused on heart health, how does what you study relate to a healthy heart? A: Many people know about the relaxing experience of floating in water or the value of taking some time each day to pause and be away from the usual hustle and bustle of daily activities. We are currently studying the potential therapeutic impact of a particular form of Reduced Environmental Stimulation Therapy (REST) called Floatation-REST, on mental health in individuals with anxiety disorders, depression, eating disorders, or substance use disorder. Floatation-REST reduces external sensory input to the central nervous system by minimizing environmental stimulation, through the act of floating supine in a pool of water saturated with Epsom salt. In this environment, the density of the salt water allows for effortless floating. The temperature of the air and water is matched to the person’s skin temperature, and visual and auditory stimulation and movement is minimized. Our research using Floatation-REST (Paper 1) (Paper 2) has shown that it can significantly reduce blood pressure during the float session, especially the diastolic blood pressure, reduce breathing rate, and certain metrics of heart rate variability, suggesting a shift in the autonomic nervous system toward a more relaxed state. Interestingly, Floatation-REST is also associated with enhanced awareness for cardiac and respiratory sensations while reducing anxiety levels in anxious individuals, indicating a paradoxical effect. We have also recently found that Floatation-REST acutely lowers anxiety and stress symptoms and improves some aspects of body image in hospitalized individuals with anorexia nervosa. Q: How do your present studies take the next steps in studying heart health as it relates to eating disorders? A: Our ongoing studies are adding to the rigor of prior research by thoroughly characterizing the cardiovascular changes induced by Floatation-REST and examining how neural and physiological changes are associated with its anxiolytic effects. For example, in healthy individuals, we have found that Floatation-REST is associated with a reduced functional coupling of brain activity within the hubs of brain networks most responsible for creating and mapping our sense of self. We also recently found that women with anorexia nervosa show reduced brain-body network connectivity after undergoing a cardiac stress challenge; the less connected these parts of the brain were, the more anxiety, depression, and negative body image the women had. We plan to extend these studies to identify whether changes in similar brain networks helps to explain the beneficial impacts observed with Floatation-REST in individuals with eating disorders. Q: Do you need people to help you with this research project? A: We are conducting several studies looking at the role of the brain-body connection in eating disorders. When an individual receiving treatment with Laureate qualifies for ongoing research studies, they may be offered the opportunity to participate. The clinical team assists in evaluating how participation will support their recovery and whether the individual might benefit from engaging in the study. We also need volunteers not in treatment for an eating disorder to help with this research. If you or someone you know between the ages of 13-40 would like to be one of our paid volunteers, please contact our lab or fill out the form on our website. |
Archives
July 2024
Categories
All
|
VISIT LIBR6655 South Yale Ave. Tulsa, OK 74136
918.502.5100 | [email protected] |
|
© 2009-2024. All Rights Reserved. Laureate Institute for Brain Research
Site powered by Laureate Institute for Brain Research















 RSS Feed
RSS Feed