|
What are the most common ways the holidays can trigger stress, anxiety, and sadness?
What can I do to minimize stress? The key word is ROUTINE, the other, CHOICES.
0 Comments
Dr. Olusola Ajilore - January 9, 2024
"Network Approaches to Precision Psychiatry" William K. Warren, Jr. Frontiers in Neuroscience Lecture 12:00 pm - 1:00 pm Program in the LPCH auditorium Dr. Ajilore is the Center for Depression and Resilience Professor in the Department of Psychiatry at the University of Illinois-Chicago. He graduated magna cum laude from Harvard University with a degree in biology. Dr. Ajilore did his MD/PhD degree at Stanford University where he studied the negative effects of stress hormones on the brain. His lab currently uses computational neuroimaging techniques and digital biomarkers to better track and treat neuropsychiatric disorders. Dr. Ajilore is also serves as the Associate Head for Faculty Development, the director the Mood and Anxiety Disorders Program and as a member of the National Advisory Mental Health Council for NIMH. Learning objectives:
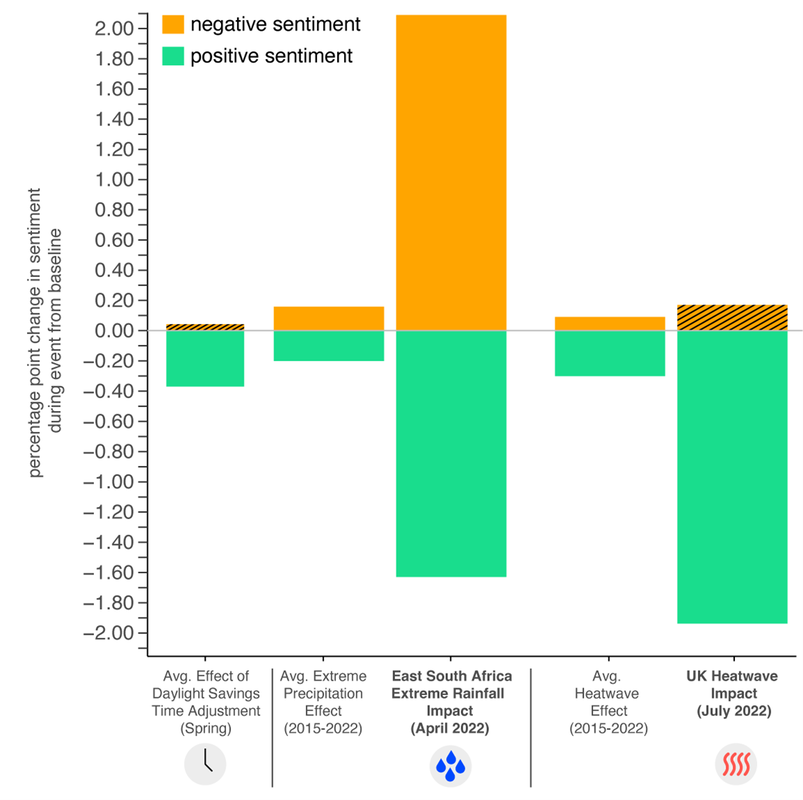
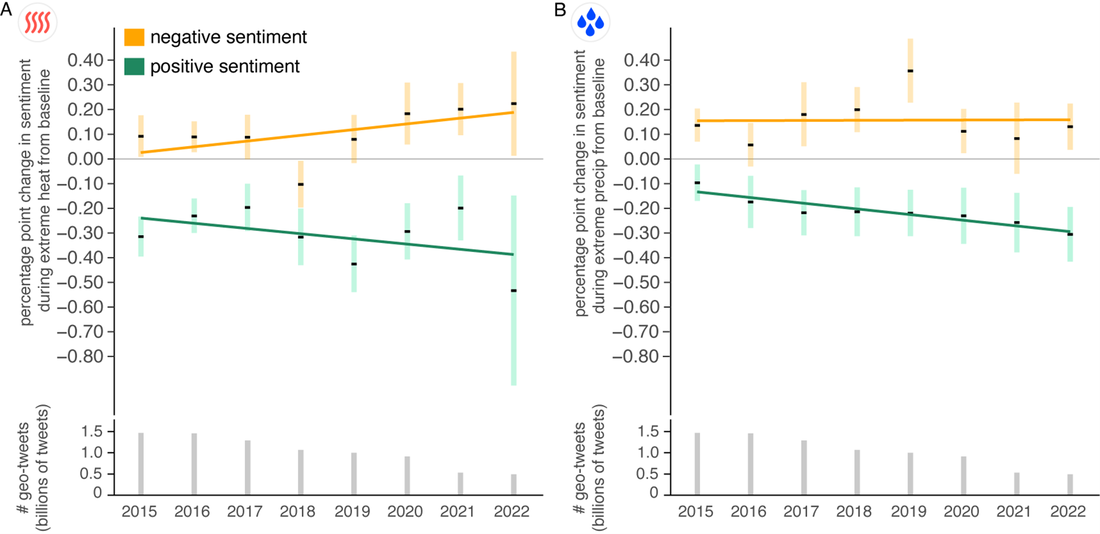
For Physicians: Saint Francis Health System is accredited by the Oklahoma State Medical Association to provide continuing medical education for physicians. Saint Francis Health System designates this live activity for a maximum of 1 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity. For Psychologists: The Oklahoma State Board of Examiners of Psychologists, the American Psychological Association and the Oklahoma Psychological Association recognize AMA PRA Category 1 credit™. Saint Francis Health System is accredited by the OSMA For Social Workers: An application has been sent to the Oklahoma State Board of Licensed Social Workers for 1 hour Category 1 Clinical. For CADCs and LADCs Saint Francis Health System is accredited as a provider of continuing education programs for CADCs and LADCs through the Oklahoma Board of Licensed Alcohol and Drug Counselors. (1 hour) The LPC/LMFT This event as been approved by the State Board of Behavioral Health Licensure (BBHL) for 1 hour of CE. For questions , email: Lauren Haguewood at lehaguewood@saintfrancis.com Dr. Nick Obradovich Contributes to Annual Health and Climate Change Report Published in The Lancet11/15/2023 Lancet Countdown 2023 Report reveals the human cost of climate inaction Dr. Nick Obradovich at the Laureate Institute for Brain Research has contributed new findings presented in the eighth annual global report of the Lancet Countdown on Health and Climate Change. The report delivers a concerning health stocktake, with new global projections revealing the grave and mounting threat to health of further delayed action on climate change. “Our health stocktake reveals that the growing hazards of climate change are costing lives and livelihoods worldwide today. Projections of a 2°C hotter world reveal a dangerous future, and are a grim reminder that the pace and scale of mitigation efforts seen so far have been woefully inadequate to safeguard people's health and safety”, says Dr Marina Romanello, Executive Director of the Lancet Countdown at University College London. “With 1,337 tonnes of carbon dioxide still emitted every second, we aren’t reducing emissions anywhere near fast enough to keep climate hazards within the levels that our health systems can cope with. There is an enormous human cost to inaction, and we can’t afford this level of disengagement – we are paying in lives. Every moment we delay makes the path to a liveable future more difficult and adaptation increasingly costly and challenging.” Dr. Nick Obradovich, a contributing author to the Lancet Countdown 2023 Report and Chief Scientist for Environmental Mental Health at the Laureate Institute for Brain Research said: "We know from an increasingly large body of research that environmental stressors like extreme heat, flooding, and large storms impede our physical and mental health. They simply make it harder for us to be well, a fact we observe via our indicator on social media sentiments that decline in response to adverse climatic conditions. The broad efforts by our Lancet Countdown team to trace and monitor the myriad manners in which climatic stressors are altering human well-being represent an important undertaking. I'm pleased to be a part of this project and look forward to ever more high-quality research feeding into the process and informing the indicators and metrics we monitor going forward." Key findings from The Lancet Report
The failure to seriously mitigate climate change is self-evident in the report, with health-related losses and damages soaring globally. However, the report is launching ahead of the 28th UN Conference of the Parties of the UNFCCC (COP28), which will – for the first time – feature health as a key theme, with an official Health Day and a climate-health ministerial. The Lancet Countdown report contributes to the evidence needed to inform the negotiations, and deliver truly health-protecting climate change action. Responding to the report publication, UN Secretary-General, António Guterres (who was not involved in writing the report) says, “We are already seeing a human catastrophe unfolding with the health and livelihoods of billions across the world endangered by record-breaking heat, crop-failing droughts, rising levels of hunger, growing infectious disease outbreaks, and deadly storms and floods. “The continuing expansion of fossil fuels is a death sentence to millions. There is no excuse for a persistent delay in climate action. Temperature rise must be limited to 1.5°C to avert the worst of climate change, save millions of lives, and help protect the health of everyone on earth.” Find out more, and read the full report at lancetcountdown.org This report was funded by The Wellcome Trust. Q: What is this research about, and what are you hoping to learn?
A: We are doing a study to see if a special supplement, kind of like the keto diet, can change how the brain works in people with depression when performing tasks about good, bad, and personal experiences. It will take about 10-11 weeks to get all the information we need for this study. Q: Who is the ideal candidate to participate in this study? A: To be in this study, you should be feeling depressed. If you take medicine, you need to have taken the same amount for at least 6 weeks before joining the study. But don't join if you're pregnant, might be pregnant, or want to get pregnant soon. Also, if you're breastfeeding, want to take vitamins or change your diet during the study, have heart or kidney problems, another ongoing health issue, feel like hurting yourself, or are very scared of tight spaces, it's best not to be in the study. Q: What happens to people who take part in this research? A: We need up to 75 people for our study. Everyone will have a talk with a mental health expert, answer some questions, do brain games, get pictures of their brain, give blood and urine samples, and try either a special diet-like drink or a placebo for two months. Q: How do you decide who gets the keto-like supplement, and who gets the placebo? A: In this study, whether you will get the supplement or a powder that does do not anything is like flipping a coin. Half of the people will get the special drink, and the other half will get a pretend one. You and the doctor won't know which is which, but they can find out in case of an emergency. Q: Could being involved in this research hurt me? A: No, this study is low risk, but there are a few things that might not feel so great. First, the special drink could give you an upset stomach, nausea or diarrhea. Second, when they take your blood, it could pinch a little. Lastly, when you go into the machine for pictures, you might feel a bit claustrophobic or nervous. But don't worry, if anything bothers you, just tell the people doing the study, and they may be able to help you feel better. Q: I’ve never had an MRI. What’s that like? A: The brain pictures are taken with a special machine called an MRI. An MRI does not involve any radiation, unlike an X-ray. The MRI machine looks like a big metal tube with a strong magnetic field around it. You'll lie on a table that goes into the tube. It's important to stay as still as you can while the machine takes pictures. It can be noisy, so you'll have earplugs to make it quieter. You can talk to the people running the MRI, and if you want to stop, they'll help you get out. They may also keep an eye on your heart rate and how you breathe using a small device on your finger and a band on your chest, but it won't be tight. Q: Will being involved in this research benefit me? A: You might not see direct benefits for yourself in this study, but you're doing something really important. By being part of this research, you're helping us learn more about a keto-like supplement and how it affects the brains of people with depression. This information could be used to help others with depression in the future, so your participation is valuable for everyone. Q: How long will each study visit take? A: Each study visit may vary in length, but on average, it will take a few hours. We'll do our best to schedule appointments that work for you. Q: Will I need to come to the study site for every visit? A: Yes, you'll need to come to the study site for most visits. We want to make sure we can closely monitor your progress and collect the necessary data. Q: Are there any dietary restrictions during the study? A: While you're in the study, it's important to follow the instructions provided regarding your diet. You may be asked to avoid certain foods or beverages. Q: Will I receive any compensation for participating in the study? A: Yes, we'll provide compensation for your time and participation in the study. The amount will be discussed with you during the informed consent process. Q: What if I have to miss a study visit? A: If you need to miss a study visit, please let the study team know as soon as possible. We'll work with you to reschedule and make sure you stay safe and healthy during the study. Q: Will my personal information be kept confidential? A: Yes, your personal information and data will be kept confidential. We take your privacy seriously and will follow strict guidelines to protect your information. Q: How will I receive updates on the study's progress? A: You can ask the study team for updates on the study's progress, and we'll do our best to keep you informed throughout the research. Q: I’d like to talk to someone about participating in the study. What should I do? A: Excellent! Please visit our website: ONGOING STUDIES - Laureate Institute for Brain Research, or call 918.502.5100. Dr. Jennifer Felger - November 7, 2023
"Inflammation and Anhedonia in Depression: Biomarkers, Mechanisms, and Therapeutic Implications" William K. Warren, Jr. Frontiers in Neuroscience Lecture 12:00 pm - 1:00 pm Program in the LPCH auditorium Jennifer C. Felger, PhD, is an Associate Professor of Psychiatry and Behavioral Sciences at Emory University School of Medicine. Dr. Felger’s work combines basic and clinical approaches to understand the mechanisms by which inflammation affects neurotransmitters and circuits to cause depressive symptoms in patients with psychiatric or medical illnesses. Her current work is focused on testing novel dopaminergic and anti-inflammatory therapies that might reverse the effects of inflammation on corticostriatal reward and motor circuits with the overarching goal of identifying treatments that can be targeted to patients with high inflammation. Dr. Felger has a PhD in Neuroscience and a Master’s in Clinical Research from Emory, and she completed a postdoctoral fellowship at The Rockefeller University. Her research has been funded by R01, R61/R33 and R21 grants from NIMH and by foundations like the Brain & Behavior Research Foundation (BBRF), American Cancer Society, and the Dana Foundation. Dr. Felger has received early career or travel awards from research societies like the Society for Biological Psychiatry and American College of Neuropsychopharmacology, and in 2017 she was awarded the Klerman Prize for Exceptional Clinical Research from BBRF. She is on the Editorial Board of Neuropsychopharmacology and serves as Associate Editor for Brain, Behavior and Immunity. Learning objectives:
 As a postdoctoral research scholar at LIBR, Dr. Hannah Berg, Ph.D. is dedicated to investigating the brain basis of decision-making in clinical anxiety. The long-term goal of this work is to provide insights that will help clinicians deliver more effective interventions. Dr. Berg’s clinical training in the treatment of obsessive-compulsive disorder (OCD) has inspired her to develop a program of research focused on OCD and its characteristic behavior patterns. What is OCD?
OCD is a mental health disorder that affects people of all ages and walks of life, and involves a cycle of obsessions and compulsions. Obsessions are unwanted, intrusive thoughts, images, or urges that trigger intensely distressing feelings. Compulsions are behaviors an individual engages in to attempt to get rid of the obsessions and/or decrease distress. More information about OCD, as well as resources for treatment, can be found at iocdf.org. What is your research study about? We are investigating the brain basis of various types of decision-making in individuals with and without OCD. The aim of this study is to better understand how compulsive behaviors arise in some individuals but not others. How is the study being conducted? Participants will undergo an initial evaluation for eligibility. Eligible participants will be asked to complete questionnaires about their emotions and experiences, followed by a series of computer tasks involving decision-making. Brain images will be obtained using functional magnetic resonance imaging (fMRI). Why do you want to conduct this research? Treating OCD has been one of my favorite parts of my job. I am consistently impressed by the bravery and vulnerability that patients show when they enter treatment, and it is immensely rewarding to help someone experience freedom from obsessions and compulsions. However, our gold-standard treatments for OCD, including exposure and response prevention (ExRP) and medications, are only effective for about 50-70% of patients. By shedding light on compulsions, I hope that this research will lead to improved treatments for OCD. In particular, ExRP involves a detailed understanding of what a patient thinks and feels before, during, and after they engage in compulsions. To the extent that this research study can help clinicians understand the brain states and psychological states that lead to compulsions, it will lead to more effective delivery of ExRP. Furthermore, insights from this study may lead to the development of new treatments, including psychotherapies, medicines, and neuromodulatory approaches that offer relief from OCD. Are you looking for participants? We will be recruiting participants beginning in November 2023! This is a pilot study, so we plan to recruit a relatively small number of participants, including individuals with and without OCD. If you are interested in participating, you can contact our assessment team here. Several LIBR researchers will be participating as speakers in the 2023 Zarrow Mental Health Symposium "New Horizons in Brain Science" organized and hosted by the Mental Health Association Oklahoma on September 20-23, 2023. Register to attend the virtual conference here. Wednesday, September 20th, 20239:00am - 10:30am Neurobiology and Eating Disorders Speakers: Scott Moseman MD, CEDS Sahib Khalsa MD, PhD 11:30am - 1:00pm Practical and Neuroscientific Perspectives of Behavioral Therapy Speakers: Robin Aupperle, PhD Elisabeth Akeman Hannah Berg, PhD Thursday, September 21st, 202312:45pm - 1:45pm A Window Into the Depressed Brain Speakers: Leandra Figueroa-Hall, PhD, MSc, BSc Kaiping Burrows, PhD Friday, September 22nd, 202312:45pm - 1:45pm
Focused Ultrasound: An Emerging Neuromodulation Tool Speakers: Salvador Guinjoan, MD, PhD Aki Tsuchiyagaito, PhD Dr. Tsuneya Ikezu - October 3, 2023
"Microglia and Extracellular Vesicles in Neurologic Disorders" William K. Warren, Jr. Frontiers in Neuroscience Lecture 12:00 pm - 1:00 pm Program in the LPCH auditorium 11:00am - 11:45am Lunch will be served beforehand in the LPCH banquet room Dr. Tsuneya Ikezu is a Professor in the Department of Neuroscience and Director, Molecular NeuroTherapeutics Laboratory at the Mayo Clinic in Florida. Research in the clinic focuses on neuroimmune cell-mediated regulations of neuronal function, neurogenesis, neuroinflammation, and neurodegeneration. Researchers in Dr. Ikezu’s lab are particularly interested in how the innate immune-related cells, extracellular vehicles, and molecules in the central nervous system influence the pathology and progression of select neurodegenerative disorders such as Alzheimer’s disease and related disorders Prior to this, Dr. Ikezu was Professor of Pharmacology and Neurology at Boston University School of Medicine and led the Laboratory of Molecular NeuroTherapeutics for 10 years. He has authored more than 120 journal articles, which were cited over 23,000 times, edited the textbook Neuroimmune Pharmacology (Springer Nature) and served on several editorial boards. Over his career, Dr. Ikezu has received Vada Kinman Oldfield Alzheimer’s Research Award (2000), Inge Grundke Iqbal Award from Alzheimer’s Association (2016) and recently Jack Spivack Excellence in Neuroscience Award (2018). Dr. Ikezu received his M.D. and Ph.D. from University of Tokyo School of Medicine and completed post-doctoral trainings at Massachusetts General Hospital and Cleveland Clinic Foundation. Dr. Ikezu’s lab webpage: The Molecular Neurotherapeutics Laboratory at Mayo Clinic Learning objectives:
Saint Francis Health System designates this live activity for a maximum of 1 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity. For Psychologists: The Oklahoma State Board of Examiners of Psychologists, the American Psychological Association and the Oklahoma Psychological Association recognize AMA PRA Category 1 credit™. Saint Francis Health System is accredited by the OSMA For Social Workers: Saint Francis Health System is an approved provider of continuing education for social worker through the Oklahoma State Board of Licensed Social Workers for 1 hour Category 1 Clinical. (CEP Number - 20230007) For CADCs and LADCs Saint Francis Health System is accredited as a provider of continuing education programs for CADCs and LADCs through the Oklahoma Board of Licensed Alcohol and Drug Counselors. (1 hour) The LPC/LMFT This event as been approved by the State Board of Behavioral Health Licensure (BBHL) for 1 hour of CE. For questions , email: Lauren Haguewood at lehaguewood@saintfrancis.com
Tulsa, Okla. – A trailblazing study conducted by researchers at the Laureate Institute for Brain Research (LIBR) in Tulsa, Okla., has made significant strides with a novel technique for treating anorexia nervosa (AN), an eating disorder characterized by low body weight, body image abnormalities, and anxiety. The study, “The impact of floatation therapy on body image and anxiety in anorexia nervosa: a randomized clinical efficacy trial,” appears in the peer-reviewed scientific journal eClinicalMedicine, a part of The Lancet Discovery Science initiative.
The researchers identified several immediate and sustained effects of Floatation-REST (Reduced Environmental Stimulation Therapy) in inpatients with anorexia nervosa. Also known as “float therapy”, Floatation-REST is a non-pharmacological treatment that involves floating effortlessly in a shallow pool of warm water saturated with Epsom salt, in a lightproof, soundproof, humidity- and temperature-controlled environment, and it is increasingly used by the general public as a stress reduction tool. In the study, the anorexia nervosa inpatients randomized to receive floatation-REST reported immediate and repeated reductions in body image dissatisfaction and improved anxiety relative to a comparison group of anorexia nervosa inpatients randomized to receive care as usual, whose symptoms were unchanged. Moreover, the body image improvements in the floatation-REST group remained after the treatment and lasted for up to six months. “This breakthrough offers a new therapeutic direction in treating anorexia nervosa, a psychiatric disorder known for its challenging prognosis and high mortality rate,” said psychiatrist Sahib Khalsa, MD, PhD, Director of Clinical Operations at LIBR, and senior author of the study. “Anxiety is a common co-occurrence in anorexia nervosa that does not respond well to standard anxiolytic medications such as benzodiazepines,” he added. “The large anxiety reductions induced by float therapy in these patients suggest that this tool presents a potent opportunity to treat anxiety via non-pharmacological means in anorexia nervosa. Additional research is needed to examine the anxiolytic effects of float therapy in other eating disorders.” “These findings also make way for new forms of treatment for eating disorders which, in conjunction with traditional treatments, may help to alleviate diagnostic features of AN that are more difficult to treat, such as body image,” commented co-first author Emily Choquette, PhD, a clinical psychologist and postdoctoral scholar at LIBR. “The reliable and sustained effect of floatation-REST on body image dissatisfaction suggests that it may be studied as a tool to augment the effectiveness of traditional psychotherapies.” Because anorexia nervosa is a severe and persistent psychiatric disorder, the search for effective treatments is ongoing. “This study underscores the importance of continually seeking innovative approaches and broadening the horizons of existing therapeutic options,” added Dr. Scott Moseman, MD, CEDS, Medical Director of the Laureate Eating Disorders Program. “These findings may pave the way for new forms of treatment, such as float-assisted psychotherapy, which aim to further enhance the body image and anxiety improvements obtained via existing evidence-based interventions.” The research team was led by senior author Sahib Khalsa, MD, PhD, Director of Clinical Operations at the Laureate Institute for Brain Research, Director of the LIBR Float Clinic and Research Center, Associate Professor in the Oxley College of Health Sciences at The University of Tulsa, and conducted in close collaboration with psychiatrist Scott Moseman, MD, CEDS, Medical Director of the Laureate Eating Disorders Program from which the participants were recruited. Co-first authors on the study were Emily Choquette PhD, a post-doctoral research associate at LIBR, and Michael Flux PhD, a former lab volunteer and collaborator at LIBR. Additional collaborators included clinical neuropsychologist Justin Feinstein, PhD, President and Director of the nonprofit Float Research Collective. The research was supported by the Laureate Institute for Brain Research and was conducted at LIBR between March 2018 and February 2021. CONTACT: For more information about the study, contact Sahib Khalsa, MD, PhD, at Laureate Institute for Brain Research at skhalsa@laureateinstitute.org. ABOUT LAUREATE INSTITUTE FOR BRAIN RESEARCH (LIBR) Launched in 2009, the Laureate Institute for Brain Research is home to a multidisciplinary team of scientists and clinical research staff who apply neuroimaging, genetic, pharmacological, neuropsychological and psychotherapeutic methods to investigate the neurobiology and treatment of psychiatric disorders. LIBR’s creation was supported by The William K. Warren Foundation for the purpose of conducting studies aimed at developing more effective treatments and/or prevention strategies for these disorders. The studies are led by scientists from diverse backgrounds, including psychiatry, psychology, physics, cognitive neuroscience, developmental neuroscience, population neuroscience and genetics, molecular and cellular neurobiology, and computer science. |
Archives
April 2024
Categories
All
|
VISIT LIBR6655 South Yale Ave. Tulsa, OK 74136
918.502.5100 | info@laureateinstitute.org |
|
© 2009-2024. All Rights Reserved. Laureate Institute for Brain Research
Site powered by Laureate Institute for Brain Research







 RSS Feed
RSS Feed